Editor’s Note: Being able to easily assess a patient’s condition would help clinicians determine whether changes in treatment are needed. Japanese research presented at the latest annual conference of the American Society of Anesthesiologists has found that a patient pulmonary index could be a predictor of respiratory adverse events.
In the First National Survey of Patient-Controlled Analgesia Practices conducted in 2013 by the Physician-Patient Alliance for Health & Safety, 7 out of 10 hospitals (70.7 percent) would like “a single indicator that accurately incorporates key vital signs, such as pulse rate, SpO2, respiratory rate, and etCO2.”
In research presented at the latest annual conference of the American Society of Anesthesiologists, Hiroshi Morimatsu, M.D.,Ph.D (Okayama University Hospital, Okayama, Japan) and his colleagues wanted to determine whether a patient pulmonary index could be a predictor of respiratory adverse events.
Could the patient pulmonary index these researchers looked at be the “single indicator” 7 out of 10 hospitals are looking for?
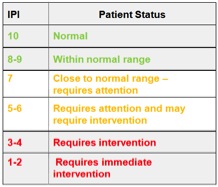
The patient pulmonary index the researchers used encompassed a patient’s end-tidal CO2, pulse oximetry, respiratory rate and pulse rate on a ten point scale as illustrated on Wikipedia below:
The study included 163 patients with a high risk for hypoventilation in the PACU after general surgery. The researchers found:
Of the 162 patients, eleven patients (7%) suffered from RAE. Among them, one patient needed re-operation and treatment in intensive care unit. The duration of PACUs was longer in patients with RAE than in those without RAE (RAE group: 97.2 ± 44.4 minutes vs. non-RAE group: 51.8 ± 27.2 minutes; p < 0.0001). Initial IPI of RAE group was lower than that of non-RAE group (6.5 ± 2.5 vs. 9.1 ± 1.3; p < 0.0001). Similarly, Initial SpO2 of RAE group was lower than that of non-RAE group (96.6 ± 4.4% vs. 98.3 ± 1.9%; p =0.0147). We finally found that sensitivity and specificity of IPI were better than that of SpO2 for onset of RAE. The area under the receiver operating characteristic (ROC) curve of IPI was 0.86 and that of SpO2 was 0.56.
The researchers concluded that the patient pulmonary index was superior to pulse oximetry alone for predicting the onset of respiratory adverse events after surgery. As Dr. Morimatsu told Anesthesiology News, clinicians should pay more attention to patients with a score of less than 7.
Please let us know about single indicators that incorporate key vital signs, such as pulse rate, SpO2, respiratory rate, and etCO2 that you have used.
PPAHS will be interviewing Dr. Morimatsu about his research. Please follow us on email or by social media to receive notice of this discussion.