By: Dr. Jasmine Bonder, DNP, MSN, ACNP-BC, RN (Head of Clinical Care, Aidaly; Board of Advisors, Physician-Patient Alliance for Health & Safety)
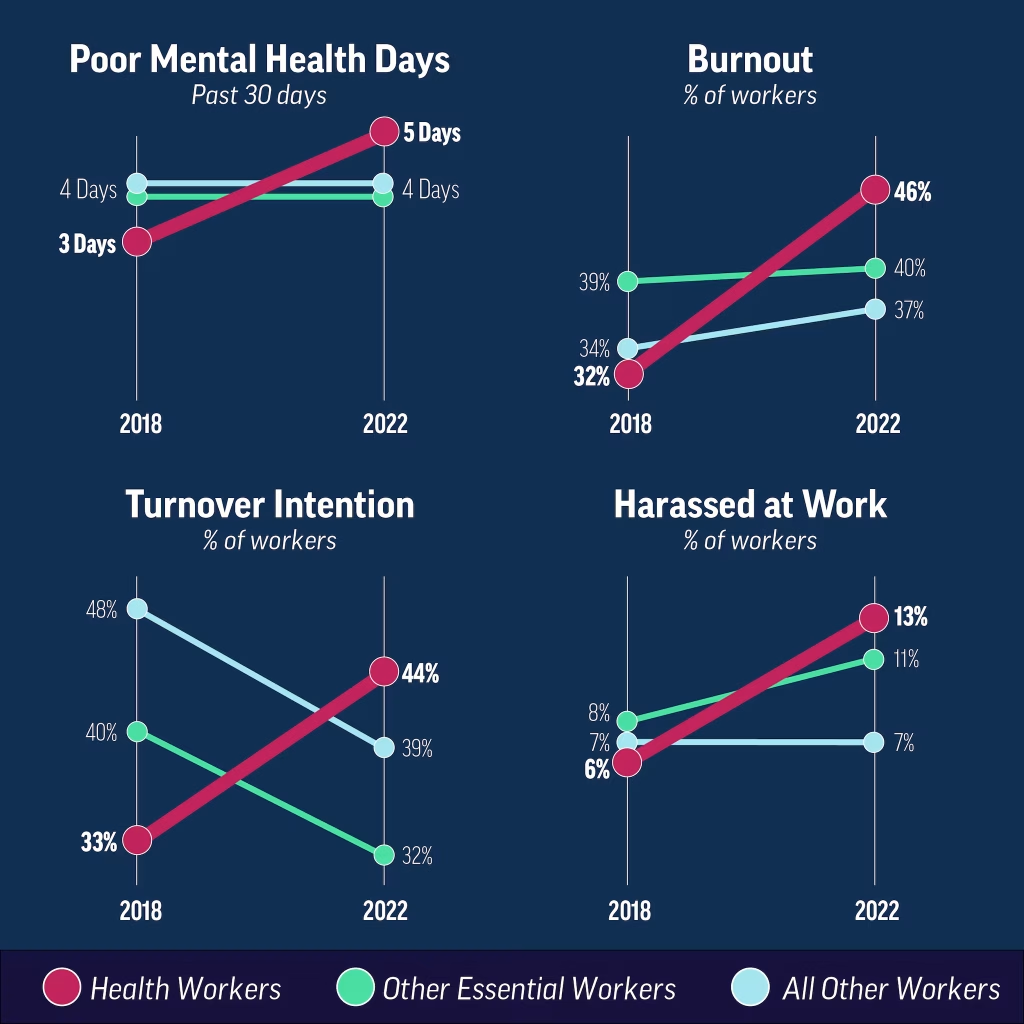
Emotional distress among healthcare providers is an increasingly pressing concern, with profound implications for their overall well-being and professional performance. According to a 2022 report by the Centers for Disease Control and Prevention (CDC), a significant 46% of healthcare workers reported experiencing burnout, a notable rise from the 14% reported in 2018. This alarming increase identifies the growing challenges faced by those in the healthcare sector, where emotional and psychological strain is more prevalent. Psychosocial hazards amongst healthcare workers have been attributed to poor and understaffed models, high acuity with minimal peer support and untrusted management systems.
The sustained emotional distress within the healthcare workforce has profound and far-reaching ramifications.The rates of emotional distress among healthcare providers were noted at the onset of the COVID-19 pandemic, and they have consistently risen since then. Dr. Tejal Gandhi, Chief Safety and Transformation Officer at Press Ganey, has emphasized the critical need to address emotional harm with the same level of urgency as physical harm. Her concerns highlight a growing recognition of the impact emotional safety has on both healthcare providers and the patients they care for.
Emotional distress has been closely linked to several detrimental outcomes, including poor staff engagement, heightened rates of burnout, and consistent turnover. When healthcare workers are emotionally distressed, they are unlikely to be fully engaged in their roles, which can lead to a decline in the quality of care that they provide. The resulting burnout exacerbates this issue, as exhausted and overwhelmed staff are more prone to errors, reduced productivity, and ultimately, leaving the profession altogether.
We propose and highlight three solutions to help combat this global concern in the health field:
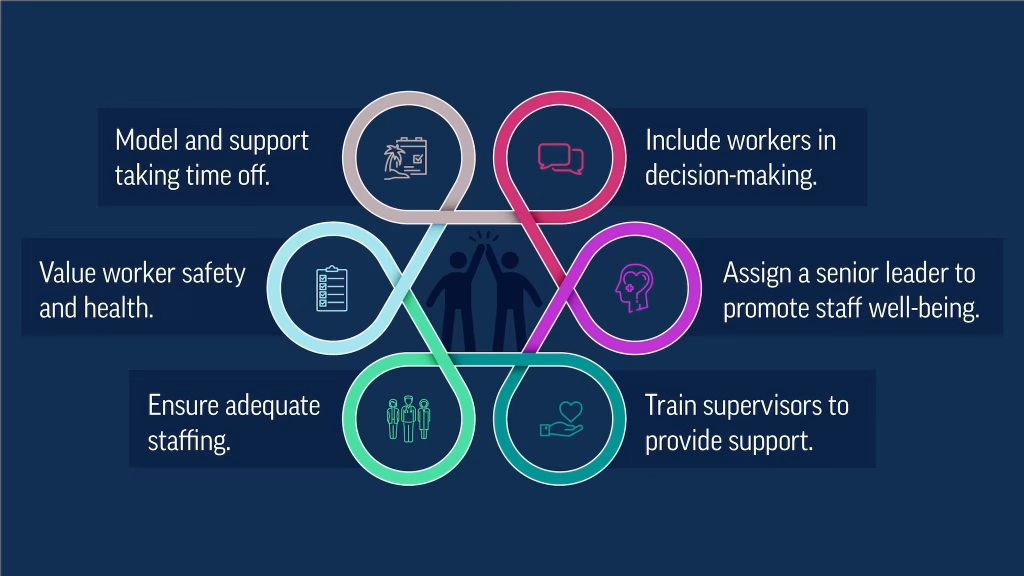
- Maintain Healthy Clinical Workloads – Assessing the clinical workloads of medical professionals is crucial to maintain a healthy balance between patient care and provider well-being. Understanding the capacity of each healthcare provider to effectively manage their workload is essential to delivering high-quality care and preventing burnout. A risk assessment that takes into account the varying levels of patient acuity can help in distributing workloads more equitably among healthcare providers. The specific needs of each patient, such as the intensity of care, frequency of interventions, and the time required to complete tasks, hospitals can assign workloads that are not only manageable but healthier for their staff members. This can help distribute even workloads, adequate resources and tangible goals to be met.
- Utilize Technology to Streamline Clinical Workflows – Hospitals and healthcare facilities must acknowledge the rapid evolution of technology and the potential benefits it offers in streamlining clinical workflows. As the healthcare ecosystem continues to advance with the integration of artificial intelligence (AI), data analytics, and enhanced cybersecurity, these tools present a valuable opportunity to alleviate the stressors that healthcare providers experience at the bedside. Ensuring that each employee is educated and equipped with these tools can have a positive impact on the work environment. Each technological advancement can effectively support clinical workflow, optimizing on care and care delivery.
- Create De-Stimulation Spaces in Healthcare Facilities – When examining hospital infrastructure, an often overlooked area is the inclusion of spaces dedicated to de-stimulation and fun. De-stimulation spaces are designed to provide a break from the constant sensory input and high-stress atmosphere of hospital and health settings. These areas offer a quiet, calming environment where staff and patients can relax and recharge, reducing stress and preventing burnout. Such spaces might include quiet rooms, gardens, or areas with soft lighting and comfortable seating, designed specifically to promote relaxation and mental well-being. Implementing a space that can help decrease stimulation post challenging hospital incidents, can help employees have a moment to mentally digest and calm emotions.
A healthy physician-patient relationship is important for optimizing patient care. Part of that healthy balance is ensuring clinicians’ emotional well-being. This includes recognizing the impact emotional distress has on our healthcare workforce. It’s imperative to take a holistic and inclusive approach by implementing emotional distress prevention models to assure the success and well-being of the healthcare workforce.
 Jasmine Bonder is a visionary healthcare leader renowned for her transformative leadership and dedication to patient-centered care. As a Certified Nurse Practitioner and a Healthcare Leader, her approach involves crafting innovative healthcare delivery systems and advocating for patient rights by leveraging her Doctorate in Nursing Practice. Jasmine focuses on innovative clinical operation, medical reimbursement strategies and care delivery models to optimize patient health outcomes. Beyond her executive role, Jasmine is an angel investor, offering financial support and mentorship to early-stage healthcare startups. Her passion for nurturing the next generation of healthcare innovators reflects her belief in the power of collaboration and continuous improvement in the industry. Her contributions have earned her numerous accolades such nominations for the Top 25 Nurses in Central Texas and Jewish Federation of San Antonio Sugerman Award.
Jasmine Bonder is a visionary healthcare leader renowned for her transformative leadership and dedication to patient-centered care. As a Certified Nurse Practitioner and a Healthcare Leader, her approach involves crafting innovative healthcare delivery systems and advocating for patient rights by leveraging her Doctorate in Nursing Practice. Jasmine focuses on innovative clinical operation, medical reimbursement strategies and care delivery models to optimize patient health outcomes. Beyond her executive role, Jasmine is an angel investor, offering financial support and mentorship to early-stage healthcare startups. Her passion for nurturing the next generation of healthcare innovators reflects her belief in the power of collaboration and continuous improvement in the industry. Her contributions have earned her numerous accolades such nominations for the Top 25 Nurses in Central Texas and Jewish Federation of San Antonio Sugerman Award.